In March 2020, as the world was bracing itself for the unknowns of a rapidly spreading pandemic, Abdoulie “AJ” Jammeh DBA, Chief of EMS at Bay Pines VA, received a call from the Director of the Medical Center. The Director had just left a staff meeting, where someone had asked a deceptively simple yet profound question: How do we actually know how clean this hospital is?
For many hospitals, this was a difficult question to answer. Cleanliness had always been a priority, but never had it been scrutinized so closely, with stakes so high. But there was an easy an answer. A year earlier, in June 2019, AJ had implemented the Walsh QA Inspector program, which meticulously tracked the hospital’s daily cleaning and inspection efforts. With a few keystrokes, he could pull up reports detailing cleaning compliance across the entire facility. It was a reassuring safeguard, a source of confidence in a time of crisis.
But was it enough?
Mr. Jammeh understood that Covid had rewritten the rules of engagement. Clean wasn’t just about being clean anymore—it was about looking clean, feeling clean, being perceived as clean. He needed to do more, not just to maintain hygiene but to instill confidence. Working alongside the Walsh team, he devised a new approach: an inspection protocol specifically targeting high-traffic, high-touch areas. It was called “Corona Virus High Touch Surfaces”. AJ realized that clean was a fact, but it was also a perception.
Every Supervisor, at least three times per shift— start, mid, and end—would inspect high-touch surfaces in public spaces. Lobbies, hallways, restrooms—places patients, visitors, and staff passed through constantly. No longer would inspections be focused on behind-the-scenes areas like patient rooms and operating theaters. Cleanliness needed to be seen to be believed.
Bay Pines’ team of 24 Inspectors took the initiative to heart. Using Walsh’s iPads to record their findings, they were everywhere—checking, conferring, ensuring that “Always Clean” wasn’t just a slogan but a visible reality. By leveraging technology, Bay Pines was able to scale from 710 inspections in February 2020 to over 3,000 per month from March through September.
Then something unexpected happened.
Bay Pines’ SHEP scores—the VA’s equivalent of the widely recognized HCAHPS patient experience scores—began to climb. In 2019, their average SHEP score for cleanliness sat at 69.6%. By September 2020, after six months of intensified inspections, that number had surged to 86.7%. A 17% jump in patient satisfaction scores. A staggering improvement.
But here’s the twist: SHEP scores measure patient rooms and bathrooms, not public areas. The Corona Virus High Touch Surface inspections focused on lobbies and hallways—areas that weren’t even part of the SHEP scoring criteria. So why did the scores rise?
This is where psychology intersects with healthcare. The answer lies in what cognitive scientists call the halo effect. When patients and families saw inspectors using hi-technology to ensure public spaces were spotless, they made a subconscious leap: If they’re this thorough with the hallways, imagine how clean my hospital room must be. Cleanliness was no longer just about eliminating germs—it was about creating trust.
And trust is powerful.
It’s worth emphasizing: SHEP doesn’t measure the actual cleanliness of a hospital. It measures the perception of cleanliness. What Bay Pines uncovered was a crucial truth—by making cleanliness visible, they weren’t just improving hygiene; they were shaping perception. And perception, as it turns out, is reality.
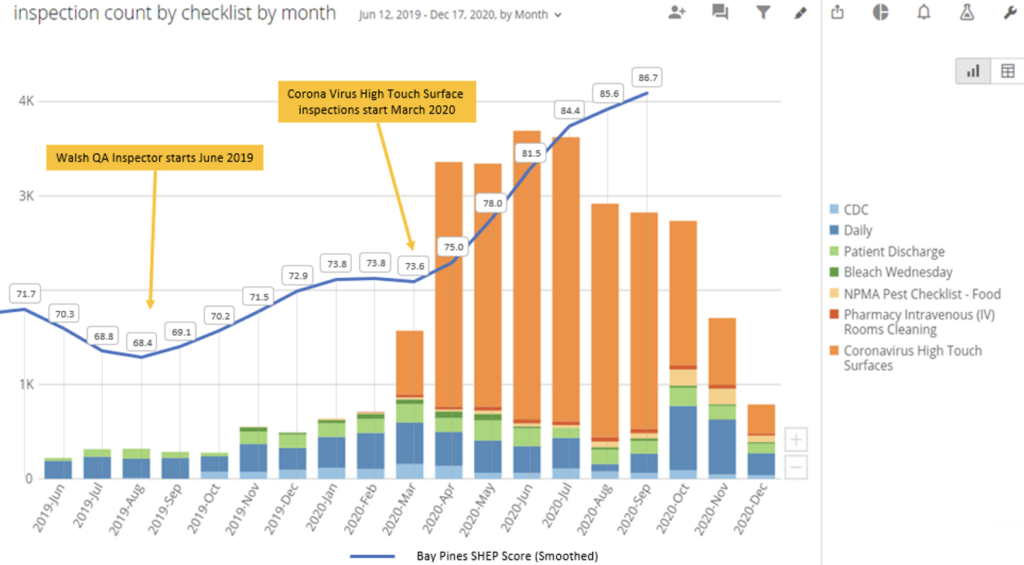
By smoothing the data, the connection becomes clear; SHEP scores increased from 68.4% to 86.7%. When plotted on a timeline, a pattern emerges: a spike in inspections is followed, about three months later, by a rise in SHEP scores. The time delay makes sense—SHEP surveys lag a patient discharge by 60 to 90 days. The increase in inspections wasn’t just a coincidence. It was a catalyst.
The lesson from Bay Pines is both simple and profound: In times of crisis, people don’t just need safety; they need to see safety. Clean isn’t just about sanitization—it’s about storytelling. And the best stories are the ones people can see with their own eyes. By showing patients and families that EMS really cares about cleanliness, perception became reality.